‘It’s a diagnosis, not a choice’: What is celiac disease?
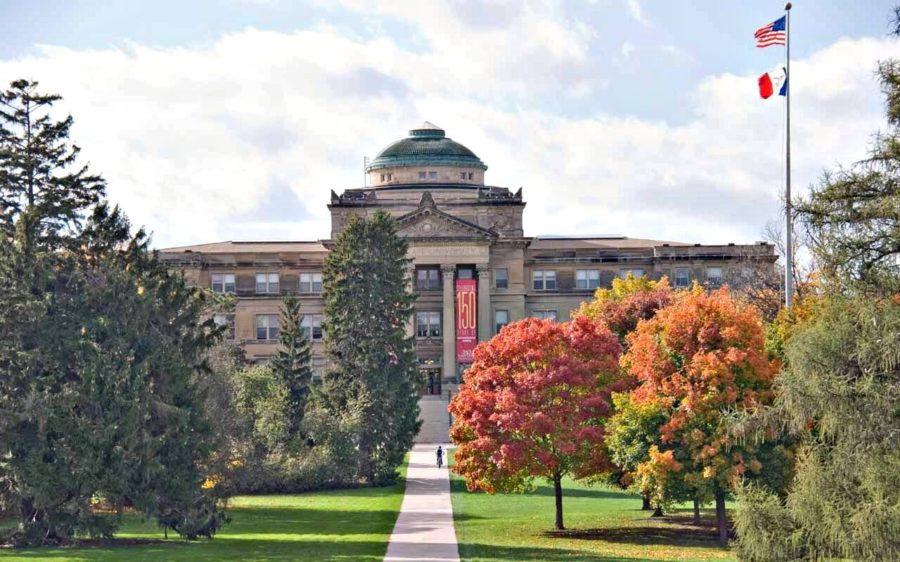
Members of Cy’s Gluten Free Friends promote the Teal Pumpkin Project inside Hy-Vee, which encourages people to put teal pumpkins on their porch for Halloween to show that they have allergy friendly treats.
February 6, 2018
For those with celiac disease, eating gluten free is a crucial part of their diet. In fact, it’s a basic health necessity.
“It’s a diagnosis, not a choice,” said Lexi Buren, senior in child, adult and family services and co-president of Cy’s Gluten Free Friends (CGFF).
Buren has been gluten free for five years, after first experiencing symptoms of her gluten allergy in high school.
“I had migraines almost every day for a year,” Buren said. “After countless doctor’s appointments, we went to see a chiropractor, and he suggested not eating gluten for a few days. The difference was night and day.”
Buren said after testing her genes with another doctor, it was confirmed. She had celiac disease.
Symptoms commonly faced by those with celiac disease when they eat gluten are stomach cramps, diarrhea, vomiting, migraines and irritability, Buren said.
The genetic autoimmune disease makes a person’s small intestine sensitive to gluten proteins commonly found in wheat, rye and barley products. This sensitivity is so acute, it damages the intestine, and makes it difficult for the body to absorb nutrients.
Where these symptoms are generally similar among members of the gluten-free community, each individual experiences their sensitivity uniquely, Buren said.
“An eighth of a teaspoon can affect some people, but I think it’s different for every person,” Buren said.
For her, eating any product made with gluten makes her throw up or develop stomach aches and migraines, Buren said.
Brittany Lende, junior in chemical engineering and CGFF member, has celiac disease, and feels similar reactions when she consumes gluten.
Unlike Buren, however, Lende’s body has been unable to tolerate gluten since she was 18 months old.
“I don’t remember finding out, only what my parents told me. I think I got sick with something, and they gave me antibiotics I reacted badly to…[then] they gave my mom a list of what I could eat, rather than what I couldn’t,” Lende said.
Since coming to Iowa State, Lende has found the diverse college community much more inclusive to her diet than she was used to growing up in Spirit Lake, Iowa, Lende said.
“Ames is really good about [having gluten-free options], and you can tell that [ISU Dining] staff are really educated about [food allergies],” Lende said.
Lende is a student who has registered with Iowa State’s Housing and Dining departments as well as Student Disability Resources to have dining accommodations because of her gluten allergy. Because of this, she can eat within the Special Diet Kitchen at Union Drive Marketplace (UDCC) in order to avoid the symptoms of accidentally consuming gluten.
“They are really good about keeping everything gluten free in the Special Diet Kitchen,” Lende said.
The Special Diet Kitchen specializes in preventing the top eight common food allergens (dairy, eggs, fish, shellfish, tree nuts, peanuts, wheat and soy) from contaminating the food of students with medically required special diets, said Nicole Wright, the interim ISU Dining registered dietitian.
Any student with medical documentation of their allergy who registers as Lende did can eat in the kitchen with no additional cost to a meal plan, Wright said.
Although they appreciate the accommodation, one criticism Lende and Buren, who ate in the Special Diet Kitchen her freshman year, have had about the service involves a desire for more variety in the gluten-free meals served.
This criticism has been met, however, by a receptive dining system, Buren said.
“Our main mission at ISU Dining is to cater to the students’ preferences and interests, and to offer a wide variety of choices. [Because of this], we have a Special Diets Food Committee that meets with students… and [we’re] adapting the menu continuously,” Wright said.
Cy’s Gluten Free Friends is a student organization that meets monthly with this special diet committee to communicate their dining preferences and suggestions, Lende said.
“[We] discuss what is going well and what could go better…We are really lucky here [with the dining services],” Lende said.
Alongside working with ISU’s dining system to make eating easier on campus for individuals with celiac disease, CGFF also serves as an outlet for information, philanthropy and fun for those in the gluten-free community, Buren said.
The club meets the first or second Monday of each month, and holds a variety of events: social events, fundraisers for celiac disease research and treatment, gluten-free recipe sharing and potlucks.
“CGFF has really helped me in knowing where to go out to eat. I wasn’t that experienced in knowing where to go, even though I’ve had [celiac disease] my whole life,” Lende said.
Buren also enjoys the advice CGFF has given her in eating out, and she hopes more places will continue to provide more options for individuals with food allergies or intolerances, Buren said.
Lende also is hopeful that the community will continue develop more gluten-free options.
“There is a good thing in [gluten-free diets] being a fad diet, and it’s that companies have been making more gluten-free products,” Lende said.
However, with growing popularity in the gluten-free diet, Buren warns against the food production industry assuming everyone ordering from a gluten-free menu is making their selection on a casual choice. Those with celiac disease are ordering to avoid foods that make them physically ill.