Editorial: The truth behind COVID-19 science
The ISD Editorial Board urges everyone to listen to the science and examine the real facts behind COVID-19.
July 6, 2020
The COVID-19 pandemic has clearly caused severe disruption to the world, but there still appears to be common debates on how to handle coronavirus and prevent the spread. A consensus doesn’t seem to exist between politicians, citizens and researchers across the country about what to do, even though there are many Americans who are hospitalized after being exposed to COVID-19.
So, what is the right thing to do? Making wise decisions is urgent in times such as these, but it is difficult to mitigate all the varying factors in order to make a smart decision. Let’s break those factors down:
Initially, it was predicted there would be a 15 percent death rate.
Later, it doubled to 30 percent, predicting a global mortality number of 250,000.
This sudden change in numbers shows how much a country should give their attention on implementing regulations immediately. This virus has been extremely dangerous and effective in spreading because there was, and still is, so little information about it.
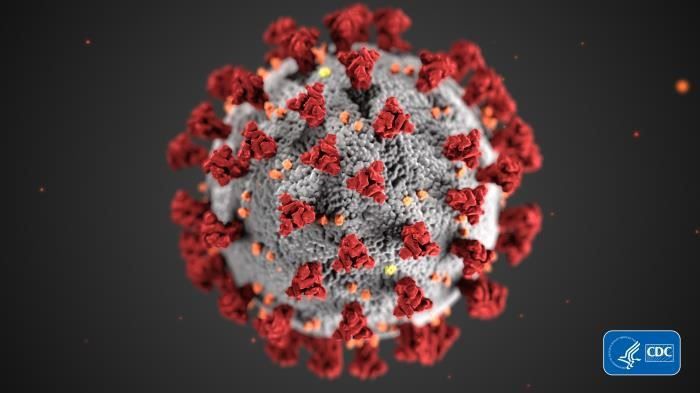
COVID-19 spreads most effectively through human respiratory droplets, which is most commonly transmitted through talking, coughing, sneezing and other similar respiratory functions.
Wearing a mask is advised to reduce the amount of respiratory transmittal, although it’s possible to contract COVID-19 by handling an infected surface. Although possible to contract COVID-19 by touching an infected surface, it is unlikely.
Wearing face masks and social distancing can indeed help stop the spread of the virus. Pandemics can be ended through these tactics, as seen in several countries around the world that have had a high peak in cases, but level off after taking action. However, the majority of experts say the only way of ending the pandemic is through a vaccine.
But are we close to finding that vaccine?
Producing a vaccine to a disease takes approximately three to six years, but scientists are working hard to accelerate the process. COVID-19 is more infectious and we have not built up community immunity yet. The reason a vaccine is so important is that it doesn’t just protect the person who gets the vaccine, it protects the larger community by slowing the spread of the virus. That’s why it’s likely we won’t end the pandemic until we obtain a vaccine.
Researchers are in a race to develop a vaccine for COVID-19. According to the World Health Organization, 140 candidates are in the process. However, introducing a vaccine undergoes many phases.
In the preclinical stage, researchers introduce the vaccine to animals and check for immunity responses. This step was successfully completed by the University of Oxford, Imperial College London, BioNTech and many more. Fifteen companies and universities, including the University of Oxford, have attempted vaccinating a small community of volunteers in hopes to offer results to the public. Yet, none of them have been approved for general use.
These vaccines have been developed through understanding some basic COVID-19 knowledge:
According to research, Cytokine storms and T-cell counts, which originate in the bone marrow in the body, offer an idea on how to treat COVID-19. But these are still in an experimental stage.
Although there isn’t a consensus on how to deal with COVID-19, there is certainly not a consensus on one fact: COVID-19 will be around for a while.
Some predict it would change its virulence. Some researchers suggest it could become less deadly with time. Others argues it could mutate and become more fatal.
This is not just the flu and the people who perpetuate this idea are dangerous. COVID-19 has a higher hospitalization rate and is more deadly than the flu.
Be preventative. Listen to the scientists.