Research finds music therapy benefits those with Parkinson’s disease
music therapy’s effect on parkinson’s disease
October 1, 2019
Elizabeth Stegemöller, associate professor in kinesiology, stood on the John F. Kennedy Center for Performing Arts’ stage for the grand opening of the REACH — the new art facility aimed at further connecting the audience to art — and was asked to give a presentation on her research.
Stegemöller and her team have conducted research on the effects of music therapy in patients with Parkinson’s disease for six years. Her research covers the gamut of symptoms such as gait, finger tapping, stress and singing. Through the years she has expanded the field as well as developed lasting relationships.
The concept of music therapy is not new to the world of science, but Stegemöller and her fellow researchers’ work on its effects on Parkinson’s disease doubled the number of papers published on the topic. Stegemöller’s research mainly focuses on singing, but she has studied finger tapping, motor control and gait in the past.
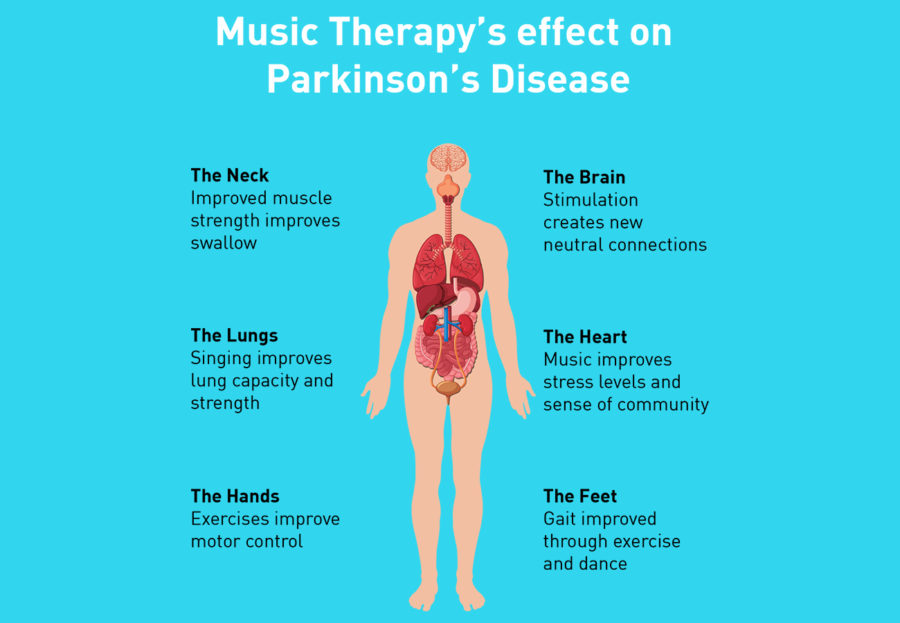
According to Stegemöller, music therapy works in many different ways. First, music increases the brain’s ability to make new connections. Increasing the amount of dopamine, an essential transmitter molecule in the brain, is one of the main ways music therapy works. Listening to preferred music automatically increases this chemical, and music therapy stimulates it in desired regions of the brain.
Rhythm in music improves the creation of connections by causing the neurons in the brain to fire at the same time. Harmonic structures in the music help reduce the amount of confusing information your brain takes in from the outside world. The final process utilized in music therapy is the use of music to stimulate certain parts of the brain to improve certain functions. These five things, according to Stegemöller, are what make her work possible.
“As a music therapist you can think that you could tweak what parts of the music you want to use to target specific parts of the brain or brain regions,” Stegemöller said. “If you wanted you could just use reading music to target a specific brain function. [With] listening to music, you can manipulate the music to target specific functions. You have access to the whole brain.”
According to Stegemöller, one of the leading causes of death in people with Parkinson’s disease is complications from swallowing. Her singing groups implement choral and vocal exercises that are proven to improve muscles used for swallowing and the respiratory system.
“We have the vocal exercises that we do, the vocal and breathing exercises and then we have the group singing,” Stegemöller said. “We actually think they are playing two separate mechanisms. Vocal exercises and breathing exercises, we think those are what are contributing to the improvements in respiratory control and the swallow.”
In her study on the subject, “Experiences of Persons with Parkinson’s disease Engaged in Group Therapeutic Singing,” her initial study included lip buzzing, glissandos, crescendos, decrescendos, articulation and group singing. Each of these musical devices built upon muscles and new mental connections. The exercises saw many of the subjects improve their ability to talk and swallow.
Her research had some interesting results outside of talking and swallowing that changed the trajectory of her research yet again.
“What we have found is that after one hour of singing, their motor symptoms — we are talking things like tremor, gait, things that are not related at all to singing — are significantly improved,” Stegemöller said. “Not directly related to singing. We were like, ‘Wow, that is kind of amazing!’”
When Stegemöller began a group in Ames six years ago, the participants did not want to leave the community they discovered. The initial study proved that singing in a group setting benefits the patients’ mental status and stress levels. To continue their research, they switched to focus on measuring this new variable.
“We know in Parkinson’s disease, if you stress them out, their symptoms are going to get worse,” Stegemöller said. “So now we are reducing their stress and improving their motor symptoms. The next question then becomes why do we see this.”
Apart from the science, Stegemöller, her students and the participants in the program have become a small community in Ames. Even though her program has grown to include four groups, she and her students develop friendships with the participants and each other.
“Every week is a great memory,” Stegemöller said. “I would say some of my favorite memories are when we as a group, when someone can no longer attend our group, we try at certain times of the year to go out and visit them and sing with them. That is just kind of a special time.”
Looking to the future, Stegemöller works with groups from around the U.S. and as far as Australia and England to one day provide the Parkinson’s disease community with a large scale study on music therapy. In Ames, her work has shifted to uncovering music therapy’s effect on inflammation in the brain. She has no intention of stopping her work as a music therapist.
“I am always very forward as I am a music therapist and I have a Ph.D. in neuroscience. I am a music therapist,” Stegemöller said. “The whole reason for why I am doing this is because I wanted to know how music therapy works. I will be an advocate until the day I die. As long as the profession wants me to be an advocate for them I will be an advocate for them in whatever way I can.”