Research Park company gets Ebola contract
October 15, 2015
An ISU Research Park company is in the unique position to manufacture a vaccine for a deadly virus.
The Ebola virus was first recognized almost 40 years ago and came to the attention of the general public in spring 2014 when an epidemic struck West Africa. The hype has since died down amidst common conversation, but the virus lives on.
NewLink Genetics, a biopharmaceutical company in Ames, was awarded $18 million from the federal government at the beginning of October to scale-up the manufacturing process relating to the investigational Ebola vaccine candidate rVSV-ZEBOV, according to Dr. Charles Link, CEO and chief scientific officer at NewLink.
He defined NewLink as a commercial entity that does basic science work, with an ultimate goal of getting drugs approved for patients in need.
“[At NewLink] when you wake up in the morning, you know you’re going to be working on stuff that really matters for people,” Link said.
NewLink originally licensed the vaccine from the Public Health Agency of Canada in 2008. NewLink was already five years into research and development of the vaccine when the outbreak struck in 2014.
The 2014 outbreak caused the vaccine to go into clinical testing much more quickly, speeding up the process by six months, Link said. He added that if they hadn’t been working on the vaccine for five years prior to the outbreak in west Africa, the company wouldn’t be in the position it’s in now.
“I always felt that it was important for humanity to see this product,” Link said.
Bioprotection Systems Corporation, a subsidiary corporation owned by NewLink, does defense contracting. They began work on the product to potentially protect against bioterrorism involving the Ebola virus.
“You never know, Ebola could be used as a threat. We have lots of imagination and so do terrorists. You just really don’t know,” said Marit Nilsen-Hamilton, professor in biochemistry/biophysics and molecular biology.
Link said he had a feeling the vaccine was something they should work on.
NewLink has since licensed the vaccine to Merck & Co., a large-scale manufacturing company that has the means for large-scale production. Merck is one of the top two or three largest vaccine manufacturers in the world, according to Link, and he sees partnering with them as very important.
Link said the CEO at Merck previously worked with civil rights in South Africa, so Merck was excited to get involved in NewLink’s product.
“We’ve had a great relationship with them and it’s worked seamlessly,” Link said.
The company is working toward a vaccine that is practical to different social and environmental conditions. Link said Merck has a lot of experience converting vaccines that have to be stored at a frozen temperature into vaccines that can be stored at room temperature.
“That’s important in the third-world when you don’t have access to cold storage,” Link said.
The whole project is set up so no one at NewLink or Merck profits off the third-world, Link said.
“We think that’s just the right thing to do,” he added.
The $18 million in funding going to NewLink came from the Biomedical Advanced Research and Development Authority of the United States Department of Health and Human Services. The award is in addition to an initial $30 million contract awarded to NewLink in late 2014, Link said.
Before that, an $8.1 million subsidiary was awarded to NewLink in late September from the Defense Threat Reduction Agency of the United States Department of Defense. This funding is also for various developments of the rVSV-ZEBOV Ebola vaccine. This $8.1 million comes with a possibility of receiving an additional $5.2 million in the future, Link said.
The money will be used for safety testing, conformance testing and immunological testing, Link said. In laymen’s terms, the money will be used to do four things: show how effective the vaccine is, ensure the effect is consistent, ensure the vaccine is consistent and to test the activity and stability of the vaccine when produced on a large scale.
Nilsen-Hamilton, a researcher herself, said that a lot of the money that goes into research is simply to pay for people’s time. She said that in this case, money goes to organizing people who are willing to be vaccinated, getting samples, testing the samples, measuring how effective the vaccine is and then doing statistical analysis. All of that takes time, expertise and large expenses.
Link said that all their efforts are working toward getting the vaccine approved by the Food and Drug Administration. He added that NewLink has already tested the vaccine on over 10,000 people.
“Personally, it’s one of the most satisfying projects that I’ve ever been involved in in my professional career,” Link said. “No one cared about this product, and we kept it alive and nurtured it and grew it.”
Results indicate rVSV-ZEBOV might have high levels of efficacy and safety in preventing Ebola virus disease, according to an article from The Lancet, a United Kingdom medical journal, which predicted the vaccine will most likely be effective at the population level when delivered during an Ebola outbreak.
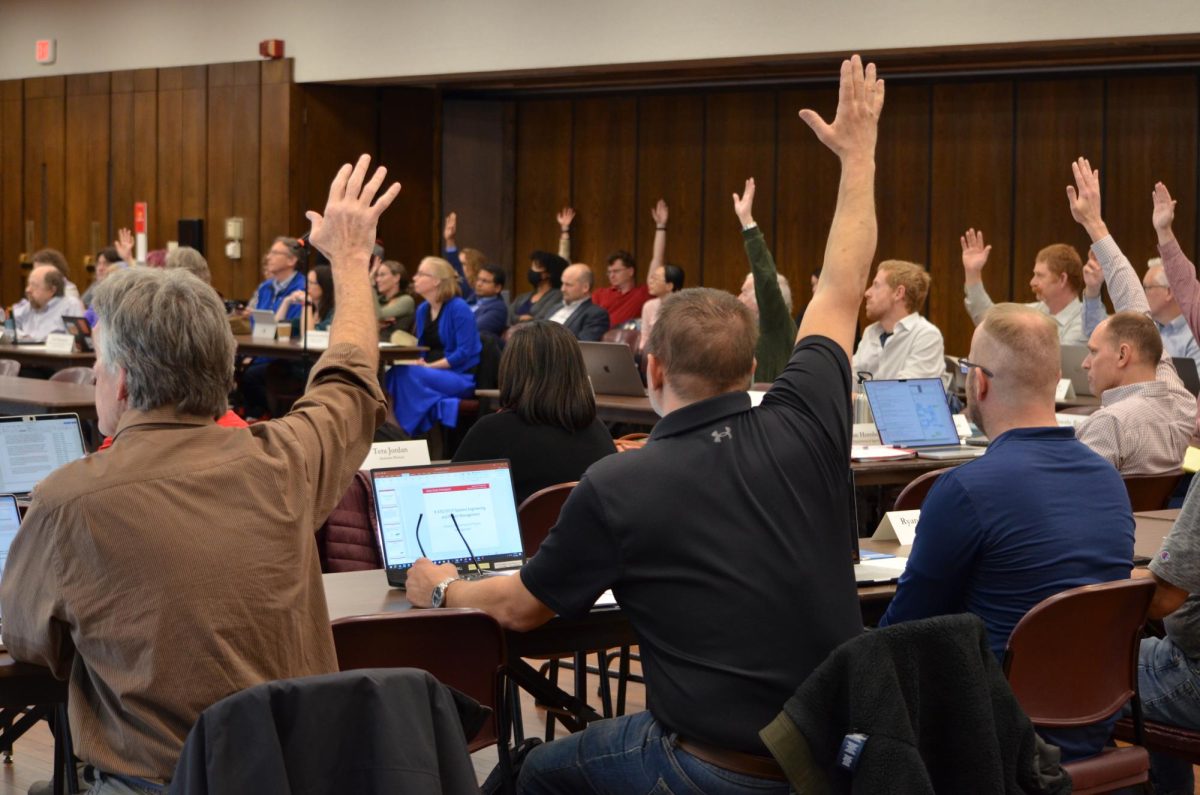
On Tuesday, Forrest Nutter, professor in plant pathology and microbiology, gave a seminar on Ebola to a group of 25-30 attendees.
Ebola was first recognized in 1976 in the Sudan and the Democratic Republic of the Congo, Nutter said, but the Ebola virus really came into the public eye during the spring 2014 outbreak.
West Africa experienced a majority of the Ebola outbreak with 3,804 total cases in Guinea, 10,672 cases in Liberia and 13,941 cases in Sierra Leone, as of Oct. 5, 2015, said Nutter. He added there have been a total of 9,649 deaths between the three countries.
Outside of west Africa, there have been 33 total cases of Ebola and 15 deaths, according to Nutter.
There were four cases of Ebola in the United States, two of which came from west Africa, he said. Nutter added that the most famous case was a man who came into Dallas and infected two nurses. He would later become the first and only case of death from Ebola in the United States.
Nutter said the number of infectious people grew exponentially between March 2014 and March 2015, but the Ebola epidemic died down eventually.
From experience, it’s known that people with Ebola can become immune because those who survived the outbreak were helping other sick individuals, Nilsen-Hamilton said, adding the immunity of various viruses and diseases varies.
That being said, there’s still more than enough cause to continue research and development on the vaccine candidate.
“There’s always going to be the chance of another outbreak,” Nilsen-Hamilton said.